Many years ago, long before the COVID-19 pandemic upended everything and turbocharged the antivaccine movement beyond anything any of us had ever seen or predicted, the central conspiracy theory of the antivaccine movement (as I like to call it) was that vaccines caused autism, and the CDC and FDA were covering up the evidence. In retrospect, that version of the central conspiracy theory seems almost quaint compared to the current version centered around COVID-19 vaccines (particularly mRNA vaccines), in which antivaxxers claim that these vaccines are killing, sterilizing, and inducing “turbo cancers” in millions, but the CDC and FDA (plus, Anthony Fauci) covered up the evidence that was apparently so obvious that experts missed all the signals that people with no training in medicine, epidemiology, or vaccinology could find. Back then, after having been a blogger for a couple of years, I had come to dread April, at least when it came to antivaccine misinformation. The reason was simple. April is National Autism Awareness Month, and I could always count on the antivaccine movement to ramp up its misinformation linking a combination of the MMR vaccine, “too many vaccines too soon,” and mercury from the thimerosal preservative that used to be used in a number of childhood vaccines before 2001 as the cause for the “autism epidemic.” Sure, often the vaccines were not the only thing blamed for rising autism prevalence. Often processed foods, wifi, and a number of other supposed “causes” were thrown in as well, but always at the center of causes that conspiracy theorists blamed for the increasing prevalence of autism were vaccines.
You might think that this whole strain of antivaccine “thought” (if you can call it that) might have disappeared to insignificance, with the rise of “new school” antivaxxers focused mainly on COVID-19 vaccines. However, as I’ve described a number of times, there is increasingly little daylight between “old school” MMR/thimerosal-autism antivaxxers and “new school” COVID-19 antivaxxers, as the latter have started repeating exactly the same tropes as the former and started to generalize their fear of COVID-19 vaccines to all vaccines. As I perused my feeds of antivax websites and blogs and came across an article by Cynthia Nevison on Robert F. Kennedy, Jr.’s website entitled In New Autism Report, CDC Again Fails to Address Root Causes, I had flashbacks to 15 years ago and couldn’t help but think that antivaxxers were partying like it was 2009. (I admit that I couldn’t find a way to slip 1999 into this quip and so had to settle for a decade later. No one ever said that I could be as funny as Clay Jones or Jonathan Howard.) I also recognized that name as someone whom I had first encountered in 2012, when she co-opted the language of scientists and skeptics to liken “autism epidemic denialists” to climate science deniers who refuse to accept the science of anthropogenic climate change characterized by global warming. At the time, she was an atmospheric research scientist at the University of Colorado, but in the meantime she appears to have become a full-time crank.
The reasons my thoughts went this way was because, in antivax-speak, “root causes” always mean vaccines, primarily at least. However, changing times do lead to changing language. For example, I couldn’t help but immediately notice how Nevison cleverly never actually uses the words “vaccine” or “vaccination” anywhere in her article and also now echoes attacks on public health organizations like the CDC for being too “woke” in that the blurb for her article states:
In its latest autism report, the Centers for Disease Control and Prevention continues to focus on equity, rather than causation, even though the new prevalence numbers have turned the equity argument upside down.
Of course, RFK Jr., being RFK Jr., and The Defender, being The Defender, the game had been given away the day before in an article by Brenda Baletti entitled 1 in 36 Kids Have Autism, CDC Says — Critics Slam Agency’s Failure to Investigate Causes. In this case, “critics” mean antivaxxers, and “causes” again mean vaccines, plus a lot of other “environmental” factors, but, make no mistake, Baletti is talking mainly about vaccines:
As autism rates skyrocketed among U.S. children over the past several decades, along with concern among parents, much research has turned to investigate the role of environmental risk factors in compounding underlying diverse genetic factors.
Environmental risk factors include metals like aluminum and mercury in vaccines, glyphosate exposure, use of acetaminophen during pregnancy and infancy, heavy metals in baby food and other organic environmental pollutants.
Studies also link industrial chemicals, such as lead, arsenic, copper, selenium, iron and magnesium, to the disorder.
Seeing this narrative, I remembered that it’s been five years since I last wrote about autism prevalence and how the antivaccine movement tries its hardest to blame its increase on vaccines. That’s why I think an update is definitely in order.
Times change, but the antivax autism narrative doesn’t
Going back over my posts on this blog and my not-so-super-secret other blog, I found that antivaxxers were flipping out over vaccines as a cause of autism in 2018 (when the CDC reported autism prevalence was reported to be 1 in 59), in 2014 (when the CDC reported autism prevalence was reported to be 1 in 68), and in 2012 (when the CDC reported autism prevalence was reported to be 1 in 88). So did our founder Steve Novella, who wrote in 2009, 2011, and 2014 about how true autism prevalence has almost certainly been unchanged over the last two or three decades.
Rising autism prevalence dating back to the 1980s has, ever since the myth that vaccines cause autism arose in the 1990s, fueled an antivaccine narrative that there is an autism “epidemic,” which in some cases has even been called a tsunami, an intentional comparison with a devastating natural disaster that sweeps away everything. At the same time, any scientific pushback against the claim that vaccines are the cause of increasing autism prevalence would be attacked as “denial.” It is a narrative that continues, with longtime antivaccine activist Mark Blaxill having pontificated on it in an interview after he’d somehow managed to publish an article with Toby Rogers and, yes, Cynthia Nevison in a bottom-feeding peer-reviewed journal less than two years ago.
Each time the CDC releases new figures for autism prevalence, along with its analysis of those figures (publications that almost always show up near the end of March, just in time for Autism Awareness Month), antivaxxers regurgitate the same argument: “Autism prevalence is still skyrocketing! It must be environmental factors (translation: vaccines, pollution, high fructose corn syrup, heavy metals, but mostly vaccines), but the CDC is ignoring these potential causes. In fairness, no one rules out environmental contributors to autism development that can alter the risk; it would be irresponsible to do so for a condition that is as multifactorial as autism. However, the evidence, as summarized by Steve and me (and many others) is that, by far, the largest contributor to autism is genetic, a conclusion that continues to be reinforced by more recent studies, to the point that signs of autism have been detected in the fetus, with the contribution of environmental factors being estimated to be between 7%-35%, but possibly as low as zero.
Which brings us to the CDC report and how autism prevalence can still be increasing even if the condition is primarily heritable; i.e., genetic. To set the stage, I will simply repeat something that I have repeated many times. Autism prevalence is referring to the fraction of children in the population given a diagnosis of a condition known as autism. As I have also discussed many times. many conditions are underdiagnosed, and that was almost certainly the case with autism decades ago continuing into recent years, but less so.
The CDC report and the antivax reaction
As the it has done periodically for a number of years now, on Friday the CDC published a report in MMWR, Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2020. As is also usually the case, the report covers up to around two or three years ago, because that’s how long it takes the data to mature into usable statistics. As the CDC does when it publishes these figures, it used data from Autism and Developmental Disabilities Monitoring (ADDM) Network, an active surveillance program that provides estimates of the prevalence of ASD among children aged 8 years.
Before I discuss the results, I’m going to stop a moment to point out a phrase: Active surveillance. We often discuss the difference between passive and active surveillance systems when discussing the Vaccine Adverse Events Reporting System (VAERS) database, a passive surveillance system, compared to systems like the Vaccine Safety Datalink (VSD), an active surveillance system. The difference between an active and passive surveillance system is that, in contrast to passive surveillance systems that rely on reports generated by healthcare workers and other sources (in the case of VAERS anyone can report), active surveillance systems are set up to monitor for a diagnosis. In the case of the VSD, the electronic health records (EHRs) of a number of large healthcare systems are monitored to look for associations between vaccination and adverse events, diseases, and health conditions. In the case of ADDM:
In 2020, there were 11 ADDM Network sites across the United States (Arizona, Arkansas, California, Georgia, Maryland, Minnesota, Missouri, New Jersey, Tennessee, Utah, and Wisconsin). To ascertain ASD among children aged 8 years, ADDM Network staff review and abstract developmental evaluations and records from community medical and educational service providers. A child met the case definition if their record documented 1) an ASD diagnostic statement in an evaluation, 2) a classification of ASD in special education, or 3) an ASD International Classification of Diseases (ICD) code.
In this study, children included in the report were born in 2012 and lived in surveillance areas of the 11 sites during 2020. Using a definition of autism spectrum disorders (ASDs) described in depth in the article, the authors then estimated the prevalence of ASDs and then:
Prevalence was calculated as the number of children with ASD per 1,000 children in the defined population or group. Overall ASD prevalence estimates included all children with ASD from all 11 sites. Prevalence also was stratified by sex and by race and ethnicity using both the U.S. Census postcensal population estimates as well as the National Center for Health Statistics postcensal bridged race denominators. The Wilson score method was used to calculate 95% CIs. Pearson chi-square tests were used to compare proportions, and the Mantel-Haenszel (Woolf) test of homogeneity compared prevalence ratios across sites. Permutation tests were conducted to test differences in medians. Cochran Armitage tests were used to detect trends in prevalence across SES tertiles. Prevalence estimates with a relative SE >30% (and ratios calculated from those estimates) were considered to have limited statistical precision and were suppressed. Statistical tests with p values <0.05 and prevalence ratio 95% CIs that excluded 1.0 were considered statistically significant. R software (version 4.2; R Foundation) and additional packages were used to conduct analyses (12).
The report also divided cases into children who had an ICD code for an ASD diagnosis only, those who had eligibility for school services without a diagnosis, and those who had a diagnosis. The key findings of the study were:
- For 2020, one in 36 children aged 8 years (approximately 4% of boys and 1% of girls) was estimated to have ASD. These estimates are higher than previous ADDM Network estimates during 2000–2018.
- For the first time among children aged 8 years, the prevalence of ASD was lower among White children than among other racial and ethnic groups, reversing the direction of racial and ethnic differences in ASD prevalence observed in the past.
- Black children with ASD were still more likely than White children with ASD to have a co-occurring intellectual disability.
A bit more detail about the first two findings:
For 2020, across all 11 ADDM sites, ASD prevalence per 1,000 children aged 8 years ranged from 23.1 in Maryland to 44.9 in California. The overall ASD prevalence was 27.6 per 1,000 (one in 36) children aged 8 years and was 3.8 times as prevalent among boys as among girls (43.0 versus 11.4). Overall, ASD prevalence was lower among non-Hispanic White children (24.3) and children of two or more races (22.9) than among non-Hispanic Black or African American (Black), Hispanic, and non-Hispanic Asian or Pacific Islander (A/PI) children (29.3, 31.6, and 33.4 respectively). ASD prevalence among non-Hispanic American Indian or Alaska Native (AI/AN) children (26.5) was similar to that of other racial and ethnic groups. ASD prevalence was associated with lower household income at three sites, with no association at the other sites.
Now let’s see how Nevison spins these results. Again, she doesn’t mention vaccines at all, but if you remember that “environmental factors” or “non-genetic factors” are code terms for vaccines you’ll get the intended message. Remember, like most antivaxxers, Nevison denies being antivaccine. Vaccines are just one of many potential genetic factors that she’s considering. In this case, though, you have to be aware of her history dating back to at least 2012 to know what she is about in her article, although the fact that she published it on the website of a longtime leader of the antivaccine movement is also a hint.
Race and autism, according to antivaxxers
The CDC report found that for the first time ASD prevalence was lower among non-Hispanic White children and children of two or more races than among non-Hispanic Black or African American (Black), Hispanic, and non-Hispanic Asian or Pacific Islander (A/PI) children. In the past, this was not true, and the lower ASD prevalence among Blacks, for instance, was attributed to less access to screening, health care, and services that led to an under-ascertainment of cases among some minorities. In other words, the difference in prevalence between white and Black children was a reflection of racial disparities. There is diagnostic substitution, a phenomenon in which children who would have been diagnosed with something other than ASD (or not diagnosed with ASD at all) are now being diagnosed with ASD.
Citing both the current report and another report by the CDC published on the same day that looked at early identification of ASD in four-year-olds, Nevison argues:
Yet one of the most notable features of both new ADDM reports is the rapid rise in ASD prevalence among racial minorities relative to white children, who historically have had the highest prevalence.
For example, in 2004, the mean Hispanic to white ASD ratio was 0.67 nationwide for children born in 2004.
In the new reports, the mean Hispanic to white ASD ratio is 1.3 for 8-year-olds and 1.8 for 4-year-olds. The mean U.S. Black to white ASD ratio is 1.2 for 8 year-olds and 1.6 for 4-year-olds.
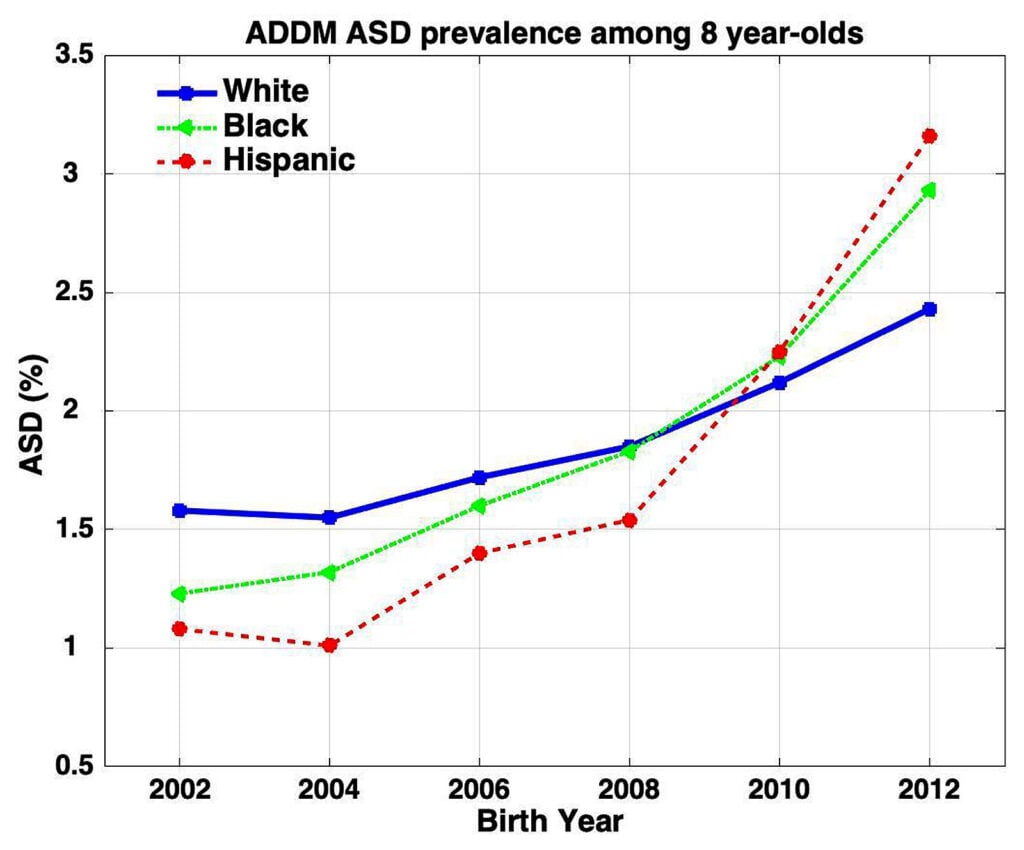
Figure 1 below illustrates how strikingly these racial differences in ASD prevalence have shifted over time. Meanwhile, absolute prevalence continues to climb for all racial groups, albeit more slowly for whites.
She even provided this figure:
How does one interpret a graph like this? First, one notes that there are no error bars. If there were, the results would look a lot less impressive, although the p-values for the prevalence ratios were statistically significant in Table 3. Now let’s see how Nevison spins this result:
The media coverage of the ADDM reports for birth years 2006 and 2008 primarily attributed increasing overall ASD prevalence to better diagnosis among Black children.
The media went so far as to imply that the overall increased rate of ASD was hopeful news because it indicated that Blacks were “catching up” to whites and achieving diagnostic equity — the hope being that their diagnosis would afford them earlier and better access to services.
The apparent underlying assumption was that there is a natural genetic level of ASD in the population, which is reflected in white prevalence, and that all races and ethnicities will eventually stabilize at that level thanks to improved outreach and screening.
The new ADDM report recognizes that, “For the first time … the prevalence of ASD was lower among White children than among other racial and ethnic groups, reversing the direction of racial and ethnic differences in ASD prevalence observed in the past.” However, the authors neglect to acknowledge that this reversal undermines the hopeful interpretation of previous ADDM data and effectively turns the equity argument on its head.
First of all, although Nevison does get the underlying assumption correct that there is likely a “natural genetic level of ASD in the population,” notice how she mischaracterizes it as being reflected in the prevalence in white children. There is no reason to assume that the same sorts differences in prevalence among different racial and ethnic groups that we observe for diseases with a large genetic component (e.g., various cancers, cardiovascular diseases) would not also be likely in a heritable condition like autism. In other words, there is no a priori reason to assume that the “natural genetic prevalence” (not an epidemiological term, but I’ll use it because it’s what Nevison uses) of ASDs would be the same in Blacks as in whites. Moreover, you can’t really even assume that there is a true difference based on one set of data. It could be that in 2 years the prevalences will be indistinguishable. In any event, whatever other factors might be influencing this increase in autism prevalence in Blacks and Hispanics, observing underserved minorities “catch up” in prevalence is actually likely an indication that these groups are finally getting access to screening and services that white children have long taken for granted.
Unsurprisingly, antivaxxers are having none of this. For example, at SafeMinds an old antivax warrior Sallie Bernard dismissed the possibility that the increase in ASD prevalence observed among Black children in the latest report is due to better ascertainment thusly:
That does not explain why their rate is higher than white children. As a group, no racial or ethnic minority here gets better assessment and diagnosis than white children, so to explain the disparity in the rate now as due to better assessment for minorities is just ludicrous.
Note the assumption there. Assessment and diagnosis do not have to be “better” in order to produce this result in a single year’s study, particularly if the actual prevalence in Black children is actually higher than it is in white children. At the very least, more temporal data points are needed even to conclude that ASD prevalence among Black children is indeed higher than it is among white children.
Next, Nevison takes on the third observation, that Black children with ASD are more likely to have a diagnosis of intellectual disability:
Instead, the report adds that, “Black children with ASD were still more likely than White children with ASD to have co-occurring intellectual disability” — as though this were a reassuring line of continuity from past reports.
However, the disparity in the rate of co-occurring intellectual disability, which is nearly twice as high among Blacks compared with whites, was an overlooked and unmentioned thorn that didn’t fit with the optimistic “catching up” interpretation of the birth year 2006 and 2008 reports.
In the new birth year 2012 ADDM report, more than 60% of the 8-year-olds diagnosed with ASD nationwide have either severe (IQ < 70) or borderline (70 < IQ < 85) co-occurring intellectual disability (37.9% and 23.5%, respectively). Among Black children, more than 75% have severe or borderline co-occurring intellectual disability (50.8% and 25.1%, respectively).
Unsurprisingly, Nevison neglects to mention a big caveat described as a limitation in the study:
Finally, the surveillance case definition of intellectual disability is not the same as a clinical diagnosis; IQ measurements in young children might lack stability and children might not ultimately receive a diagnosis of intellectual disability.
Also, there could well be other reasons for this. Indeed, in the other take on these studies by Baletti, the other possibility is acknowledged only to be dismissed:
Black children with autism were far more likely than white children to have a co-occurring intellectual disability, which the report said might stem from “underascertainment of ASD among Black children without intellectual disability.”
This is, of course, a perfectly reasonable possible explanation that needs to be considered and investigated, but antivaxxers dismiss it out of hand. Bernard, of course, tries to spin this as slam-dunk evidence for an “environmental”—cough, cough, vaccines!—cause of autism:
Now they’ve diagnosed that Black children have such a high rate of intellectual disability and borderline intellectual disability. That’s a group of people with autism that have the toughest time in life. For families, it’s so hard. And so they absolutely need more attention.
“But it doesn’t explain the social determinants of health. For that, we need environmental justice. You have to ask what are they exposed to?
Meanwhile, Toby Rogers, who is both antivaccine and transphobic, predictably spins a conspiracy theory, in which “they” are keeping The Truth from you:
The unwillingness of the CDC to even ask why these numbers are increasing is a massive ‘poker tell’ that they know but are prohibited from talking about it.
Two high-quality, multi-million dollar studies in California (Byrd et al., 2002; Hertz-Picciotto and Delwiche, 2009) both concluded that better awareness, changes in diagnostic criteria and earlier age of diagnosis only explain a small fraction of the rise in autism.
Cherry pick studies much, Toby? Steve Novella discussed at least one of those studies and its flaws back when it was published, noting that the study itself came to rather conservative conclusions that Picciotto liked to spin in press interviews as slam-dunk evidence that there must be some unidentified environmental contributor to autism and ignore studies that show that the vast majority of increases in ASD prevalence (which, when you come right down to it are differences in the proportion of children in a given population who receive an ASD diagnosis) have been driven by changes in diagnostic criteria, screening, and public awareness.
Before I conclude, I will, as I have done a number of times, answer the argument from incredulity that antivaxxers often invoke, in which they claim that changes in diagnostic criteria and/or screening can’t possibly result in such large increases in a diagnosis.
DCIS, redux
Let me return to an example I use so often whenever I encounter antivaxxers claiming that “better diagnosis” or “more screening” can’t possibly explain a huge increase in prevalence of a condition or disease: ductal carcinoma in situ (DCIS), a form of breast cancer. Well, actually, whether it’s really cancer or not is debatable, but it can clearly often be a precursor to cancer, although the percentage of DCIS lesions that progress to cancer isn’t precisely known. Be that as it may, before 1975 DCIS was a very uncommon diagnosis. Now it is very common. Indeed, back in the early 1900s, DCIS was rare because by the time it grew large enough to be a palpable mass, it almost always had become invasive cancer. Now, nearly forty years after mass mammographic screening programs became prevalent, DCIS is a common diagnosis. Indeed, approximately 40% of breast cancer diagnoses are DCIS, and a recent study found that DCIS incidence rose from 1.87 per 100,000 in the mid-1970s to 32.5 in 2004. That’s a more than 16-fold increase over a 30 year period, and it’s pretty much all due to the introduction of mammographic screening. This sort of thing should not be surprising to doctors, but apparently sometimes it is.
Unlike the case for autism, the diagnostic criteria for DCIS remained pretty stable over that 30 year period. Pathologists in the 1970s and pathologists in the 2000s would likely agree on what constitutes DCIS. The same is true for other conditions. Indeed, thyroid cancer comes to mind, a disease for which increased screening with ultrasound has led to a massive increase in the number of diagnoses of thyroid cancer, the vast majority of which are almost certainly overdiagnosis. Actually, there are issues with changing criteria for the diagnosis of thyroid cancer too. Indeed, diseases for which the prevalence is increasing often involve both increased screening and changes in the diagnostic criteria.
Another example is hypertension. Before the 1920s doctors didn’t routinely measure systolic/diastolic blood pressure ratios; so there were few, if any, cases of hypertension because doctors weren’t looking for it and didn’t know how to easily measure it. Even over the last decade, prevalence of hypertension has increased (for instance, in Canada). Perhaps a better marker for hypertension diagnoses is the percentage of adults who have been prescribed antihypertensive medications, which has skyrocketed since 1950. Of course, over that time, the definition of what constituted “hypertension” has changed markedly, to lower and lower diastolic and systolic pressures, as evidence showed that treating lower blood pressures could prevent premature death, although that trend appears to have leveled off. Amusingly, various denialists lambaste such broadening of diagnostic criteria to claim that hypertension is an “engineered” epidemic. And don’t even get me started on hypercholesterolemia.
Increasing numbers of diagnoses ≠ increasing number of people with a given condition or disease
I’d like to conclude once again by emphasizing that the increasing prevalence of a condition really means an increase in the number of people given a diagnosis associated with that condition, not necessarily a “true” increase in the prevalence of the condition. If you look for a disease or medical condition more intensively, you will always find more of it—often a lot more. Always. If this principle works for something that is diagnosed by an objective test, namely a biopsy, how much more so is it likely to be for a condition that has no unequivocal biochemical or tissue test to nail down the diagnosis, like ASDs, particularly for a spectrum of disorders whose diagnostic criteria has changed considerably over the last 30 years to be more inclusive?
None of this rules out an increase in the “true” prevalence of autism over the last few decades, but the increasing consensus is that the evidence does rule out the sort of massive increase that antivaxxers claim and then blame on vaccines. What is most likely happening is that we’re getting better and better at finding and diagnosing autism, including milder cases, to the point where the apparent prevalence of autism (i.e, the number of diagnoses) is starting to converge on the “true” biological prevalence of autism as it is defined today and that we might just be starting to see the sorts of differences in that “true” prevalence attributable to race, gender, and ethnicity that we see for many medical conditions and diseases, no vaccines needed as a “root cause” to explain.